Quick overview of liver disease symptoms
Liver disease often presents without obvious or detectable symptoms. When symptoms do appear, they may include:
- Jaundice refers to the yellow discoloration of the skin and the whites of the eyes.
- Abdominal pain and bloating.
- Swelling in the legs and ankles.
- Pruritus (Itchy skin without a visible rash)
- Dark urine.
- Light-colored stool.
- Persistent fatigue and weakness
- Nausea or vomiting.
- Loss of appetite.
- Weight loss and muscle depletion
- Bruises easily.
- Mild hepatic encephalopathy (brain impairment)
- Foul-smelling breath
- Digestive issues, especially with fats
If you notice or experience any symptoms, consult your doctor immediately and get your blood tests done.
What is liver disease exactly?
Your liver is a large, powerful organ responsible for hundreds of vital functions, including filtering toxins from your blood. Although it is well-designed for this task, its filtering role exposes it to toxins, and prolonged exposure to these toxins can lead to liver damage. Excess toxins may temporarily or permanently impair liver function.
When doctors discuss liver disease, they usually refer to long-term conditions that cause ongoing liver damage. Common causes include viral infections, toxic exposure, and certain metabolic disorders. Although your liver has strong regenerative abilities, constantly being repaired can be tiring. Over time, it might struggle to keep up.
What are the stages of chronic liver disease?
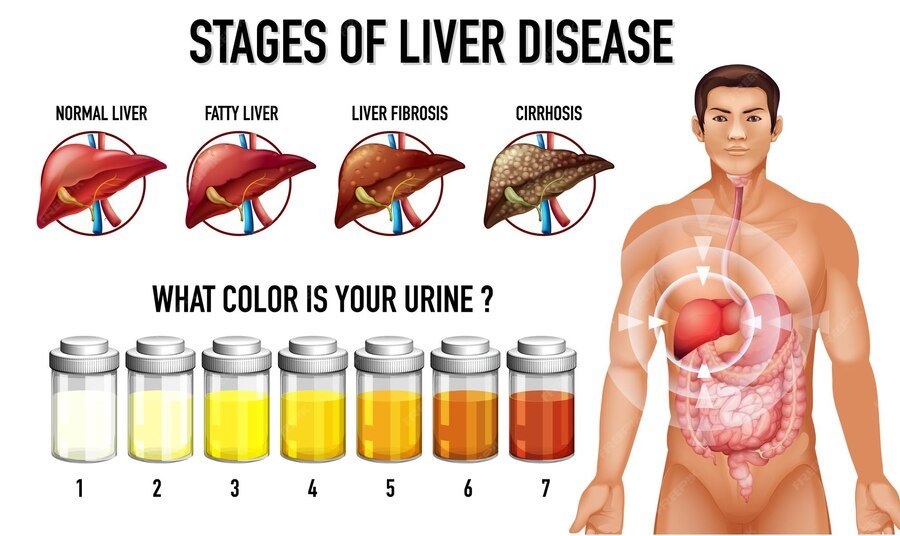
Chronic liver disease advances through approximately four stages:
- Stage 1 Hepatitis: involves inflammation of the liver tissues. This reaction happens when the liver responds to injury or toxins, trying to fight infections and promote healing.
- Stage 2 Fibrosis: involves a gradual stiffening of the liver caused by thin bands of scar tissue building up over time. This scar tissue blocks blood flow, reducing the delivery of oxygen and nutrients to the liver.
- Stage 3 Cirrhosis: involves severe, permanent scarring in your liver. At this stage, fibrosis becomes irreversible. When your liver no longer has enough healthy cells to function properly, its tissues cannot regenerate.
- Stage 4 Liver failure: occurs when your liver can no longer meet your body’s needs. This is called “decompensated cirrhosis,” meaning that your body can’t adapt to the reduced liver function.
What are the causes of liver disease?
1. Infection
Parasites and viruses can infect the liver, leading to swelling and irritation called inflammation. This inflammation hampers the liver’s normal functions. Viruses that harm the liver can spread via blood, semen, contaminated food or water, or close contact with an infected individual.
Hepatitis viruses, such as Hepatitis A, Hepatitis B, and Hepatitis C, cause the most prevalent types of liver infections.
2. Condition of the immune system
Autoimmune diseases occur when the immune system mistakenly attacks healthy parts of the body. Examples of autoimmune liver diseases include autoimmune hepatitis, primary biliary cholangitis, and primary sclerosing cholangitis.
3. Genetics
A gene change inherited from one or both parents can cause substances to accumulate in the liver, potentially damaging it. Examples of genetic liver diseases are Hemochromatosis, Wilson’s disease, and Alpha-1 antitrypsin deficiency.
4. Cancer and other types of growths
Examples of conditions leading to liver diseases include liver cancer, bile duct cancer, and liver adenoma.
5. Drug-induced liver injury
Specific prescriptions, over-the-counter medications, herbal remedies, and repeated exposure to toxic chemicals can cause liver diseases. Painkillers and fever reducers containing acetaminophen are often responsible for liver damage, especially when taken in doses higher than recommended. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, diclofenac, and naproxen can also lead to drug-induced hepatitis. Additionally, medications such as birth control pills, Amoxicillin-clavulanate, and some anti-seizure drugs may contribute to liver injury.
6. Other causes
Other common causes of liver disease include prolonged alcohol use, fat buildup in the liver, also known as metabolic dysfunction-associated steatotic liver disease (formerly called nonalcoholic fatty liver disease).
What are the risk factors associated with liver disease?
Factors that may raise the likelihood of liver disease include:
- Consistent moderate or heavy alcohol consumption.
- Obesity.
- Type 2 diabetes.
- Tattoos or body piercings done with unsterilized needles or in unhygienic conditions.
- Sharing needles for drug injection.
- Blood transfusion before 1992.
- Exposure to other people’s blood and body fluids.
- Unprotected sex.
- Exposure to chemicals or toxins.
- Family history of liver disease.
How is liver disease diagnosed?

A doctor screening for liver disease begins with a physical examination, during which they check for visible signs and ask about your symptoms. They might also inquire about your diet, lifestyle, and medical history. To confirm the diagnosis, they will order lab tests and imaging scans, such as:
- Blood tests: including a panel of liver function tests, can help identify liver disease, assess its severity, and predict potential failure. These tests measure liver-related substances such as enzymes, proteins, and bilirubin in your blood. Additionally, blood tests can detect inflammation, specific diseases, or side effects, such as impaired blood clotting.
- Imaging tests: such as abdominal ultrasound, CT scan, or MRI, help visualize the size, shape, and texture of your liver. They can detect inflammation, swelling, growths, and fibrosis.
- Elastography: is a specialized imaging test that uses ultrasound or MRI technology to assess the stiffness or fibrosis in your liver.
- Endoscopy: is used when your provider needs to view the inside of your biliary tract. It involves inserting a small camera (endoscope) through your upper GI tract. The endoscope can then be used with EUS or ERCP to examine your bile ducts.
- Nuclear medicine: imaging involves a nuclear liver and spleen scan that uses a gamma camera to detect a safe radioactive tracer injected into your body. The way your liver absorbs the tracer reveals areas that aren’t functioning properly.
- A liver biopsy: is a minor procedure that involves taking a small tissue sample from your liver for laboratory testing. Usually, a doctor can collect the sample using a hollow needle. You may need this procedure to detect cancer, confirm cirrhosis, or determine the cause of liver issues.
What is the recommended approach for managing liver disease?
Certain liver diseases require specific medical treatments; for instance, antivirals are used to treat viral hepatitis, and corticosteroids or immunosuppressants are used to manage autoimmune conditions. Nonetheless, lifestyle modifications often serve as the primary approach to managing liver disease. Minimizing the liver’s toxin exposure is crucial across all types of liver conditions, particularly those linked to excess fat, alcohol, or other harmful substances.
Early detection of liver disease is crucial for effective treatment before permanent damage occurs. Sadly, many people are unaware they have liver issues until it’s too late to reverse them. If you have cirrhosis or liver failure, you might require further treatments for complications such as portal hypertension or liver cancer. The liver may not recover fully, and a transplant could be necessary in the future.
What are some ways to prevent liver disease?
Here are some ways you can prevent liver disease:
- Drink alcohol responsibly: if you choose to consume it. Moderation generally means up to one drink per day for women and up to two drinks per day for men, according to healthy adult guidelines.
- Practice safe behaviors: always use a condom during sex, choose clean and reputable shops for tattoos or piercings, seek help if you inject illicit drugs, and never share needles.
- Get vaccinated: If you are at a higher risk of contracting hepatitis, discuss with your doctor the benefits of receiving the hepatitis A and hepatitis B vaccines. The same recommendation applies if you have been infected with any hepatitis virus.
- Exercise caution with medication intake: Use prescription and other drugs only when essential. Follow the directions and adhere to the recommended dosage. Do not mix medicines with alcohol. Talk to your healthcare provider before combining herbal supplements with prescription or other drugs.
- Avoid contact with other people’s blood and body fluids: Hepatitis viruses can be transmitted through accidental needle sticks or improper cleaning of blood or body fluids.
- To ensure food safety: wash your hands thoroughly before eating or preparing meals. When traveling in resource-limited countries, opt for bottled water for drinking, hand washing, and brushing your teeth.
- Exercise caution: when using aerosol sprays by ensuring good ventilation. When applying insecticides, fungicides, paint, or other toxic chemicals, wear a mask to protect yourself from inhaling these substances. Always adhere to the manufacturer’s instructions.
- Protect your skin: by wearing gloves, long sleeves, a hat, and a mask when handling insecticides and other toxic chemicals to prevent contact.
- Maintain a healthy weight: as obesity can cause nonalcoholic fatty liver disease, now known as metabolic-associated steatotic liver disease.
Check Liver Symptoms
Living with liver disease
Your liver plays a crucial role in your overall health, and when it becomes ill, it can impact you in numerous ways. However, you might not realize the effects of liver disease until it’s already advanced. To protect your liver, it is essential to know what can harm it and try to avoid those things. Regular health checkups can also help detect liver disease early. If you notice any symptoms or signs, it is advised to contact your doctor immediately.
Frequently asked questions
Can liver disease be reversed?
Liver disease can be reversed early on if you and your healthcare team effectively identify and manage the underlying cause. This largely depends on the cause and its treatability. After cirrhosis develops, the existing scarring cannot be reversed; however, further damage can be prevented or slowed. Chronic liver failure, however, is not reversible, although it may take years to develop.
Can liver disease be treated?
Many liver diseases are treatable. Toxic and alcohol-related conditions often improve after exposure stops. Adjusting diet and lifestyle can help manage non-alcoholic fatty liver disease. While some liver diseases are not curable, they can usually be controlled with medication. Certain inherited, autoimmune, and viral liver diseases may need lifelong management.
What steps can I take to lower my risk of liver disease?
To lower the risk of liver disease, get vaccinated against hepatitis A and B when available. Practice good hygiene by washing your hands after using the bathroom, handling food carefully, and using needles safely to minimize the risk of infection. Drink alcohol in moderation and follow medication instructions. If you have substance use disorder (SUD), seek treatment to prevent toxic hepatitis. Additionally, manage metabolic risks, such as blood lipids and sugar levels, with guidance from a healthcare provider.
When is it necessary to see my doctor regarding my liver?
If you notice ongoing symptoms of liver disease mentioned earlier, see your doctor. Seek emergency care if you observe yellowing of your skin or eyes (a sign of liver stress or deterioration); become extremely drowsy, confused, or excessively sleepy; vomit blood or notice black stools (which may suggest severe bleeding in your food pipe or stomach); develop a high fever with chills; experience shortness of breath; notice significant abdominal swelling; or suddenly have stomach pain or fever.
How can I look after myself while managing liver disease?
If you have liver disease, support your liver health by maintaining a balanced diet rich in whole foods, plants, and lean proteins. Monitor your body mass index (BMI) with your healthcare provider’s guidance to maintain a healthy range. Avoid alcohol, tobacco, and over-the-counter medications, and seek advice from your provider to help you quit. Take medications as prescribed and consult your healthcare provider before starting any new medications. Protect yourself from infections through good hygiene and safe sex practices to lessen additional liver strain. Keep up with healthcare appointments and routine screenings to catch and manage any complications early.


